What is "TPIAT" Surgery?
The TPIAT surgery is a complex operation requiring the involvement of a variety of medical professionals and scientists.
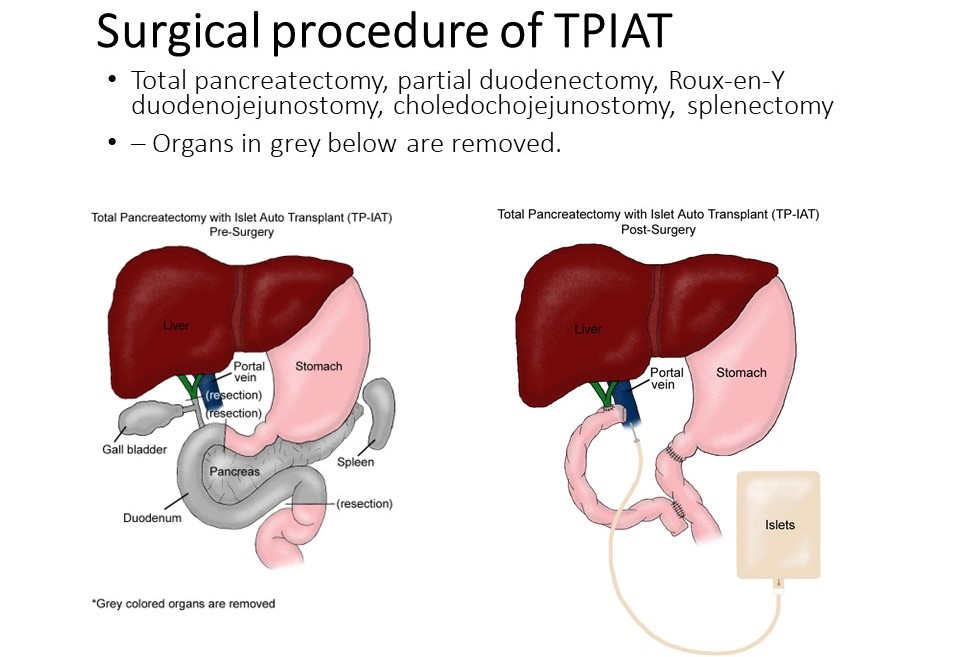
There are two main procedures that occur as part of the operation:
Total pancreatectomy: First, a surgeon removes the pancreas, spleen, and some of the duodenum (part of the small intestine). The spleen and part of the intestine are removed because removing the pancreas also resects some of the blood vessels that are shared between the pancreas and surrounding structures. The bile duct from the liver is also separated from the pancreas duct. Once the pancreas is removed, the GI tract is reconnected (most commonly with a procedure called "Roux en Y") and the bile duct from the liver is reconnected to the intestines.
Islet isolation and islet autotransplant: Next, while surgery is occurring, a special team of trained scientists will isolate the islets from the pancreas. A typical 'healthy' pancreas has around 1 million islets, which are clusters of the cells that make insulin and other hormones, scattered throughout the pancreas. A person with pancreatitis often has far fewer islets because of damage to the pancreas from the pancreatitis. The process of isolating the islets involves putting a special enzyme solution into the pancreas to dissolve the collagen connections that hold together the islets and the digestive pancreas, and then mechanically breaking apart the pancreas in a special chamber. The islets are collected and sent back to the operating room the same day, where they are transplanted usually by infusing them into the blood vessel that goes to the liver, called the portal vein.
After surgery, the islets need to send chemical signals to the liver to make new blood vessels and form their new 'home' in the liver. We call this islet engraftment. This process takes several months. During that time the medical team will work closely with you to keep your blood sugars near normal so that the islets are not under too much stress, and will have the best chance possible for survival.
TPIAT Candidacy
A TPIAT is not the right approach for everyone who has pancreatitis.
Evaluation Process for Pancreatitis at the University of Minnesota
Before a patient is considered a candidate for TPIAT at the University of Minnesota they meet with a team of doctors and other medical providers and undergo a series of tests. Each patient has a nurse coordinator who will help guide them through the process and synthesize the information from various providers.
Most patients will have the following during their evaluation:
Consultation with various medical providers including a surgeon, endocrinologist, dietician, social worker. Some individuals will see gastroenterology, pain management, and a genetic specialist, depending on their needs.
Blood work to check the function and health of their pancreatic islets, liver and kidneys.
Nutritional assessment and enzyme (elastase) measurements to check the response of the pancreas to food.
Some individuals will also have:
Imaging such as computed tomography (CT), magnetic resonance imaging (MRI) or ultrasound.
Endoscopic ultrasound (EUS) or endoscopic retrograde cholangiopancreatography (ERCP) to examine their pancreatic and ductal anatomy, or to treat strictures or stones in the biliary or pancreatic ducts.
Genetic testing to check for risk factors for pancreatitis
Additional diabetes evaluations like wearing a continuous glucose monitor.
Recovery from TPIAT
Recovery from TPIAT is a long process, often taking a full year after surgery to recover. In the first few months after surgery, expect frequent follow up with doctors, and frequent communications with your nurse coordinator. Weaning pain medication can take months. Everyone will leave the hospital on insulin therapy and this often needs frequent dose adjustments in the first 3 months. Only about 30% of individuals without diabetes before surgery will come fully off insulin after surgery, and insulin is weaned very slowly over 6-12 months. Nutrition is monitored very closely after surgery, including using a feeding tube for the first couple of months, adjusting pancreatic enzymes once oral diet is started, and monitoring vitamin and nutritional studies. Many patients will feel also feel fatigued.
Staying in Minnesota During Recovery
When patients have TPIAT surgery, they are only in the hospital for 1.5-3 weeks typically, but they remain in Minnesota for outpatient care for approximately 8 weeks post-operatively. This is for a couple of reasons: It allows for the frequent follow up appointments that are required to provide optimal care; and it allows for quick access to the emergency department and hospital in the event of a surgical complication.